What Is Diastasis Recti?
Diastasis recti is the thinning and stretching of the connective tissue (linea alba) that lies between your 2 rectus abdominus sheets (6 pack muscles). This is something that happens naturally as your belly expands during pregnancy and close to 100% of women who carry full term will get some amount of separation.
During the first 6-8 weeks postpartum, a lot of healing will naturally occur. For about 1/3 to 1/2 of postpartum women (depending on which study you look at), they will still have a “gap” after the first 8 weeks postpartum. At that point, healing your diastasis recti is going to require some intentional rehab and strengthening work.
Rehabbing and strengthening your core is important in postpartum so you can avoid problems down the road and truly feel your best. In fact, even if you don’t have diastasis recti, I still recommend that you spend some time strengthening your core and body after birth!
It doesn’t matter if you are 3 weeks postpartum or 1 year postpartum, I still recommend that you self-assess for diastasis recti if your provider hasn’t done it for you.
Watch the video below and have a piece of paper and pen ready to write down your findings! You can re-assess every 4 weeks or so.
More Than Just The Gap
Here’s a myth buster for y’a?
Diastasis recti is so much more than just the “gap” (or how many fingers wide) between your 6 pack muscles.
The gap is wayyy less important than the integrity or density of the tissues.
Having a gap between your six pack muscles DOESN’T automatically = dysfunction or weakness.
However, if you can dig down pretty deep into the tissues and there seem to be a lot of slack or loss of integrity, rehabbing and strengthening would be recommended.
There are lots of factors that could contribute to Diastasis Recti. Some may be in our control while others aren’t.
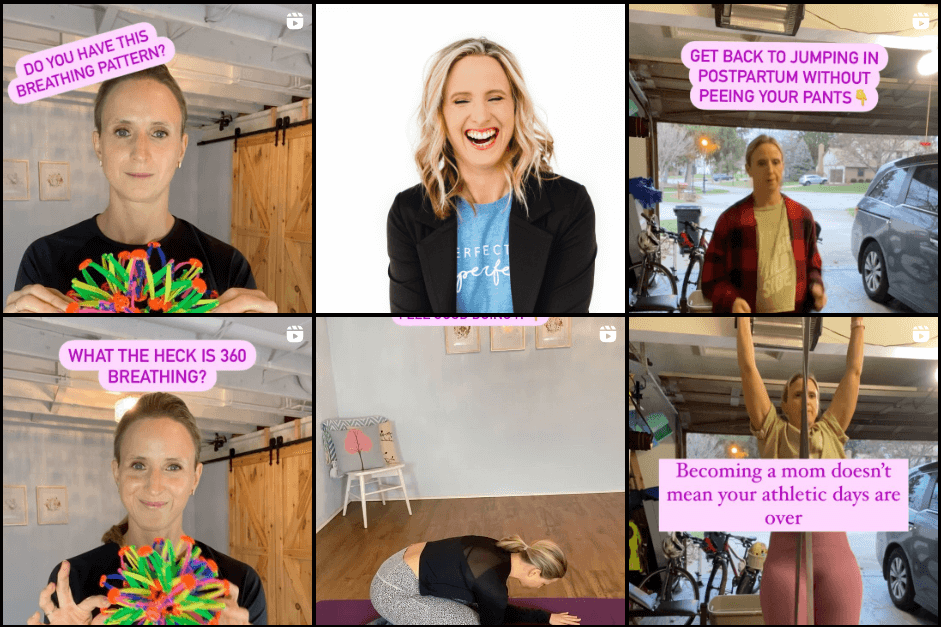
Here are 3 things that I teach to all my clients that can help minimize their risk of DR during pregnancy and help them heal it postpartum.
- 1️⃣ Better Breathing Mechanics aka getting that rib cage moving!
- 2️⃣ Posture and Alignment to support their deep core system
- 3️⃣ Appropriate Exercise Selection to support their body right now and not worsen separation
There’s a lot of misinformation on the internet about Diastasis Recti (often called DR, DRA, or abdominal separation) and I want to help you know the facts!
Did your provider check for Diastasis Recti at your 6 week postpartum visit? Comment below and let me know! I’m seriously curious?.
When I work with a postpartum client, we always do a DR check to start and assess where their core strength is. I look for the separation between the muscle bellies, the tension of the tissues and the depth. I also like to assess in different positions and check how the person responds with different core exercises.
If we don’t test things out, we won’t know where you should be starting with your rehab and strengthening journey?♀️.
Why Getting Your Rib Cage Moving is Crucial to Minimize or Heal DR
Your core canister is a pressure system (think of it as a can of pop/soda/fizzy). The top of the canister is your diaphragm (your main breathing muscle), the bottom is your pelvic floor, the front is your abdominal muscles, and the back is your back muscles.

The #1 way we can minimize Diastasis Recti is by learning how to manage intra-abdominal pressure and not letting too much pressure go right in the front (ab wall) where tissues might already be weakened (stretched) from pregnancy and postpartum.
If your rib cage isn’t moving much, it will impact where the pressure will go (potentially down onto your pelvic floor or out in the front of your abdomen).
Getting your ribs to move anteriorly (front), posteriorly (back), and laterally (sides) will help distribute the pressure and allow your diaphragm, abs, and pelvic floor to work more efficiently together. This is what we call 360 degree breathing!
Here’s a Reel I made recently that shows what NOT to do when practicing 360 breathing.
How Alignment Can Impact Diastasis Recti
I believe there is no perfect posture but if you’re stuck in 1 posture all of the time and you can’t ever get out of it-that could be making your ab separation worse.
For example, if you are stuck in an extension pattern or “scissor pattern” (ribs thrusting upward and pelvis tilted forward), your ab wall will constantly be in a lengthened position and it will be harder to manage pressure.
On the opposite of the spectrum, if you are stuck in a “sway back” posture (pelvis tilted posteriorly and rib cage behind your body), it will also be harder to manage intra-abdominal pressure. Your core canister (pressure system) functions best when things are stacked (ribs over pelvis).
Working on variability and finding a stacked position during pregnancy and postpartum can be really helpful in managing intra-abdominal pressure and improving movement quality. The stack is something I work on with all my clients! Fill out my 1:1 Online Coaching/Programming Interest Form if you want to work personally with me.


0 Comments